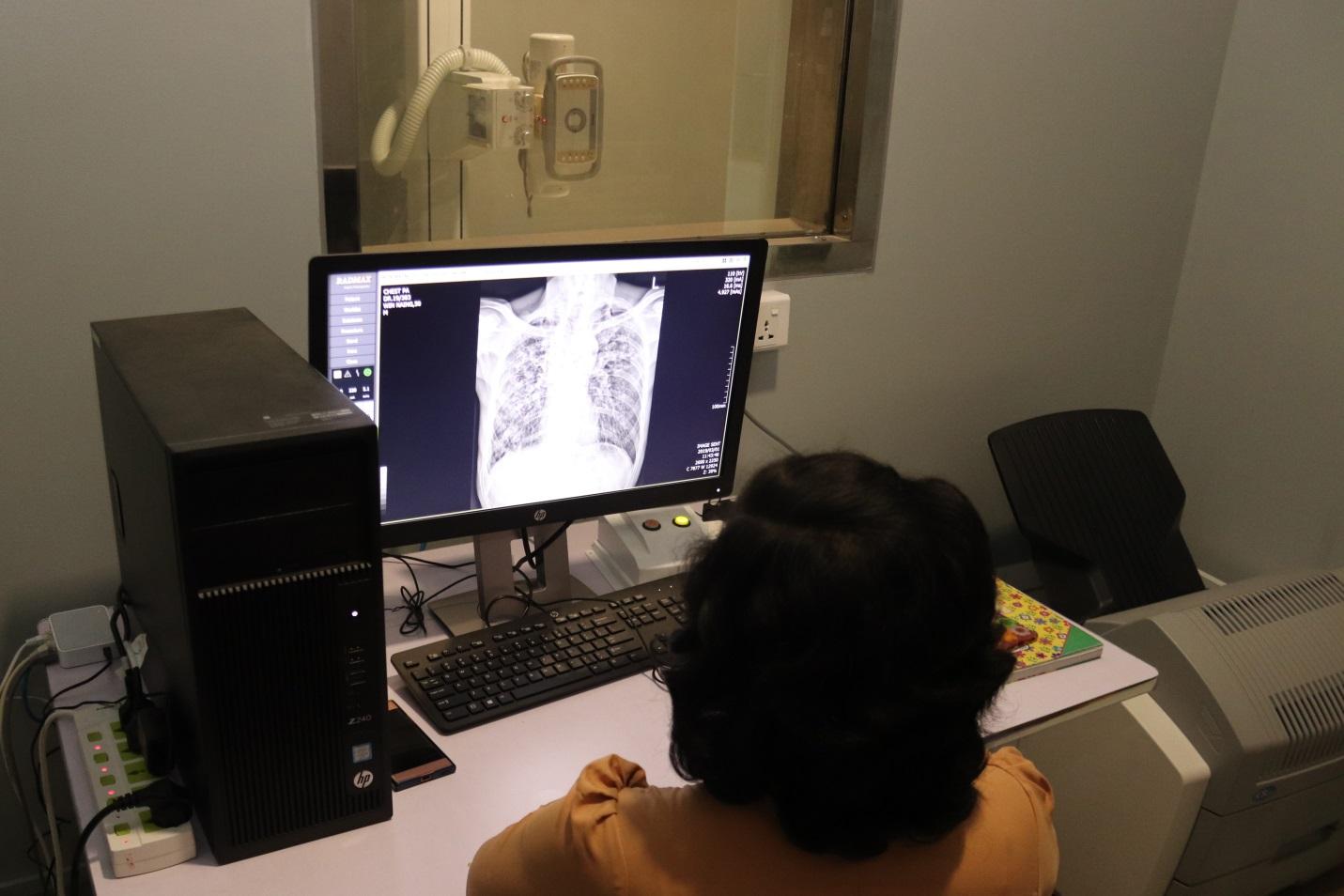
Doctor Aye Thidor Kyaw reviews test results and check chest x-rays for the characteristic spots that may indicate tuberculosis, before giving the patient a diagnosis and treatment plan.
The world’s deadliest pandemic is a disease of the poor and disadvantaged. Mycobacterium tuberculosis tends to attack the lungs of the malnourished, people who have contracted HIV or developed diabetes, or those who are working or living in cramped conditions. More than half of Myanmar’s multidrug-resistant tuberculosis (MDR-TB) is notified in Yangon, and the vast majority of cases originate in one of four townships on the fringes of the city: Insein, Mingaladon, Hlaingthaya – with its industrial zone and squatter camp – and Thaketa. In Insein, you also find the country’s leading institutions for TB diagnostics, treatment and care.
Radiographer Daw Aye Sandy Kyaw takes chest x-rays to diagnose tuberculosis at the Yangon outpatient department in Insein Township. The OPD’s x-ray machine was supplied by the Global Fund.
“We have the capacity to test up to 150 people for TB per day”, says Doctor Myat Myat Moe at the Yangon TB outpatient department (OPD) in Insein Township in Yangon. The OPD is located a stone throw away from Aung San TB hospital and the national TB laboratory. The majority of patients live in Yangon, but some also travel from other parts of the country, as the OPD is known as one of the country’s leading TB facilities. The OPD is the first stop for people who have started coughing, are experiencing night sweats, weight loss, fever or fatigue. The majority come to the OPD two to four weeks after they first started experiencing symptoms of TB, according to Doctor Myat Myat Moe. Here, they are registered, have their sputum tested and chest x-ray taken before a doctor gives them their diagnosis. Some patients leave the OPD with a chest infection diagnosis, but many do test positive for TB.
“There is still some stigma attached to getting a TB diagnosis, and some patients become depressed, especially those with multidrug resistant TB”, says Doctor Myat Myat Moe. If there is suspicion of drug-resistance, the OPD is equipped to test resistance to the drug Rifampicin, one of the most powerful first-line antibiotics used to treat TB.

Medical Technician Daw Lin Wah Thein is inserting a sputum sample into a Genexpert machine. Genexpert performs a molecular test that detects TB bacteria and resistance to Rifampicin. Genexpert can provide test results in less than two hours. The Global Fund is providing cartridges and other consumables for TB testing to the OPD in Insein, and has also procured and installed a number of Genexpert machines in other health care facilities throughout Myanmar.
The new TB OPD, as well as a Biosafety Level 3 laboratory, is the result of a long partnership between the National TB Programme, UNOPS-PR and the 3MDG fund. Both facilities were inaugurated on 24 March – World TB day – 2018. UNOPS-PR procured and installed state-of-the-art laboratory equipment, while 3MDG financed and oversaw the construction of both facilities in line with global technical standards for infection control.
In Myanmar, the Global Fund’s most significant contribution to combat TB is ensuring a continuous and sufficient supply of drugs, both for sensitive and resistant TB. Up until 2013, Myanmar had long waiting lists for MDR TB treatment, with patients waiting for months on end for the final diagnosis and dying while waiting for their turn. Now, with drugs fully available and good access to modern equipment to detect and confirm the disease, coverage of TB care is close to 100% and patients can access diagnosis and treatment very quickly. The latest TB prevalence survey shows a 46% reduction in TB prevalence in the country over the past 10 years.
The new biosafety Level 3 laboratory – which was fully equipped by the Global Fund – lays a stone’s throw from the OPD. Biosafety level 3 is necessary when working with bacteria that may cause serious diseases if inhaled, such as TB. The lab in Insein was designed, constructed and equipped according to high international standards to obtain Biosafety Level 3. This includes restrictions on airflow and air filtering, features to ensure containment, as well as sinks and eye washes that can be used hands-free, and much more. The lab itself is located behind two sets of self-closing doors. The Global Fund fully funded for establishment of BSL 3 for TB with high tech laboratory equipment with HVAC system in accordance with the WHO guidelines which was successfully commissioned and verified by an independent third party international certified agency .
“We receive the most difficult TB samples, mostly from lower Myanmar” says Dr Ti Ti, a Laboratory Advisor. The laboratory has the capacity to process up to 200 samples per day and she is responsible for making sure the laboratory is up and running and that it is always following the strict safety procedures.
“The use of positive and negative pressure rooms is crucial to maintain infection control”, she says.

Each of the rooms in the biosafety Level 3 laboratory needs to meet pressure requirements to prevent potentially harmful microbes from spreading.The Global Fund fully equipped the laboratory’s molecular, liquid culture, incubator and sterilization rooms, as well as a wide range of additional equipment that is required for a biosafety level 3 laboratory.
The laboratory is collocated with the TB hospital, which primarily treats complex cases of MDR-TB. This includes TB patients with coinfections – such as HIV/AIDS – liver failure, people who abuse substances and those who do not have the support system that is necessary to complete the long MDR-TB treatment. Patients stay in the hospital for up to one year. According to the doctors working at the hospital, 80 percent of those who are admitted for MDR-TB and more than half of those who are treated from extensively drug-resistant TB (resistance against first-line and one of the injectable second-line TB treatments) at the hospital will now be cured.

Dr Mar Mar Htay and Dr Nway Nway Win have been to a number of Global Fund training sessions that help them in their work.
Senior Consultant TB Specialist Dr Mar Mar Htay, Deputy Medical Superintendent Dr Nway Nway Win and Senior Consultant Dr Khin Aye Myint have all worked at the TB hospital in Insein Township for a number of years. Thanks to training provided by the Global Fund, they keep their knowledge up-to-date.
“Tuberculosis is a ‘naughty’ bacteria that keeps mutating. The TB knowledge I have from medical school is not as relevant anymore,” says Dr Nway Nway Win.
They mention technical training, infectious control training, MDR management and pharmaceutical vigilance training, all facilitated by the Global Fund. After attending, they pass on their knowledge to basic health staff at all levels.
The Global Fund’s investment in Insein Township supports the National Strategic Plan for Tuberculosis (2016 – 2020), which highlights the need to expand the TB diagnostic network, particularly in Yangon and Mandalay. The strategy has a goal to end the TB epidemic by 2035, and a vision to see a Myanmar completely free of TB by 2050.