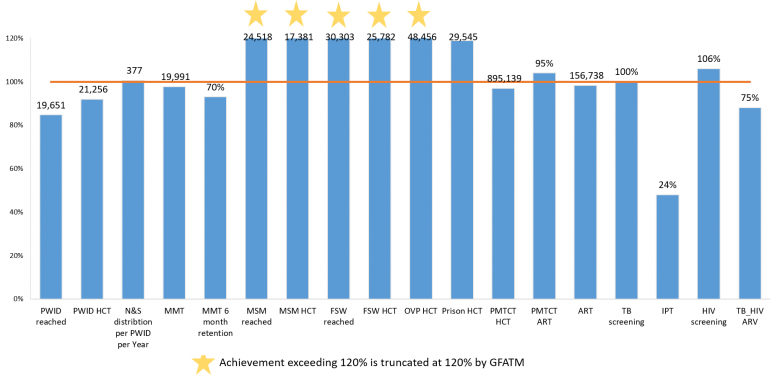
The cumulative results for 2019 are shown as a percentage of the annual target. The indicators on sex workers, men who have sex with men, and people who inject drugs reached, along with HIV counselling and testing and TB status assessed, are funded by GFATM only, whereas the others are funded by GFATM and other donors.
There has been significant progress in implementation of the HIV grant, with 10 out of 18 reportable indicators either meeting or exceeding 100 per cent of the annual target by the end of 2019.
By the end of 2019, 156,738 people living with HIV were receiving antiretroviral therapy (ART) (98% of the planned target for the year). Initiation of ART for all people living with HIV has been accelerated through ART scale-up in the public sector, with an increase in the number of ART sites to 137 and decentralized sites to 196. Increased community involvement has improved collaboration with the public sector and facilitated ART transition in terms of ART adherence and retention in care.
In 2019, 895,139 (97% of target) pregnant women received HIV counselling and testing and knew their test results, and 95 per cent (104% of target) of HIV-positive pregnant women received antiretroviral drugs to prevent mother-to-child transmission of HIV (PMTCT) provided as part of a package of antenatal care services offered to all pregnant women at public health facilities in Myanmar.
In 2019, 24,518 (Over 120% of target) men who have sex with men (MSM), 30,303 (120%) female sex workers (FSW) and 19,651 (85%) people who inject drugs (PWID) were reached with HIV prevention services.
In total, 25,782 (120%) FSW and 17,381 (120%) MSM underwent voluntary HIV testing and received their test results and post-test counselling. During the year, 21,256 (92%) PWID consented to HIV testing and received their test results.
At the end of 2019, 19,991 (98%) PWID had been enrolled into methadone maintenance therapy (MMT) in 71 MMT sites across the nation, and 70 per cent (93% of target) of persons who enrolled in MMT continued the treatment for at least six months. The MMT programme has been functioning well with the integrated services for PWID under one roof, adopting a one-stop-shop model at 11 MMT sites.
The services provided under the one-stop-shop model include MMT; HTC; ART; targeted information, education and communication and condom programming for PWID and their sexual partners; testing and vaccination for hepatitis B; prevention, diagnosis and treatment of tuberculosis; testing for hepatitis C; and diagnosis and management of sexually transmitted infections.
In terms of needle and syringe distribution to PWID, the equivalent of 377 (101% of target) needles and syringes per person were distributed in 2019.
In 2019, 48,456 (120% of target) of other vulnerable populations (OVP) consented to HIV testing and received their test results and post-test counselling.
During the year, 24 per cent (48% of target) of new HIV-positive patients started isoniazid preventive therapy (IPT).
Some 75 per cent (88% of target) of people living with HIV who had TB coinfection had been enrolled on ART by the end of the year.
During the year, 98 per cent (100% of target) of HIV patients were screened for TB in their last visit, and 95 per cent (106% of target) of TB patients had their HIV status assessed and documented.