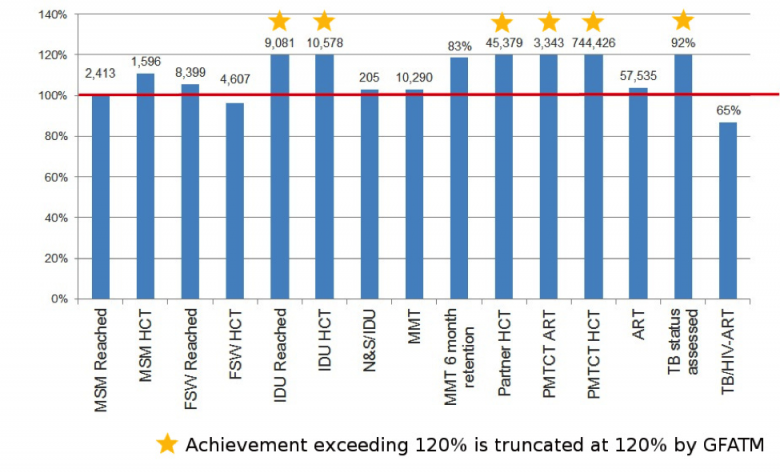
The cumulative results for Year 5 (NFM) are shown as a percentage of the annual target. The indicators on sex workers, men who have sex with men, and people who inject drugs reached, along with HIV counselling and testing and TB status assessed, are funded by GFATM only, whereas the others are funded by GFATM and other donors.
There has been significant progress in implementation of the HIV grant, with 14 out of 15 reportable indicators either meeting or achieving more than 100 per cent of the annual target by the end of 2015.
The antiretroviral therapy (ART) programme has been on an upward trend of coverage nationally and is providing quality services due to the sustained commitments and support from the Government, the Global Fund and many other development and technical partners.
By the end of 2015, 57,535 people living with HIV were receiving ART (103% of the planned target for the year). ART services had expanded and there were 82 ART centres and 101 decentralized sites nationwide.
Similarly, prevention of mother-to-child transmission of HIV (PMTCT) services were expanded to cover 309 townships across the nation. In 2015, 744,426 pregnant women received HIV counselling and testing and knew their test results, and 3,343 HIV-positive pregnant women received antiretroviral drugs to prevent mother-to-child transmission of HIV. There has been an increase in uptake of HIV testing services and an increase in the acceptance rate among pregnant women, which reflects the success of the PMTCT programme with more community involvement.
An increased level of awareness and openness has enabled key populations to come forward and take up HIV services. In 2015, 2,413 (101% of the annual target) men who have sex with men, 8,399 (105%) female sex workers and 9,081 (121%) people who inject drugs were reached with HIV prevention services.
Prevention programmes for sex workers and their clients include peer education and community outreach along with demonstration of condom use and referral for HIV counselling and testing. The 100% Targeted Condom Promotion programme (TCP) was implemented in various locations in line with the national 100% TCP framework.
In total, 4,607 (96.3%) female sex workers and 1,596 (111%) men who have sex with men underwent voluntary HIV testing and received their test results and post-test counselling. Uptake of testing has been improved by the availability of a confirmation HIV test at the same site and two-way referral linkage between prevention services and care, treatment and support services.
During the year, 10,578 (120%) people who inject drugs consented to HIV testing and received their test results. This increase is due to the introduction of integrated services under one roof for people who inject drugs, adopting a one-stop-shop model whereby testing can be done in drop-in centres combined with intensified awareness activities.
In 2015, 45,379 (120%) clients/partners of individuals belonging to key populations consented to HIV testing and received their test results and post-test counselling. This is due to a strengthening of the HIV counselling and testing programme, scaling it up to reach a greater number of intimate partners of individuals belonging to key populations.
In terms of needle and syringe distribution to people who inject drugs, the equivalent of 205 (103%) needles and syringes per person were distributed in 2015.
At the end of 2015, 10,290 (103%) people who inject drugs had been enrolled into methadone maintenance therapy (MMT) in 41 MMT sites across the nation. This opioid substitution therapy programme also includes distribution of condoms, access to counselling, HIV testing and psychosocial support, provided in collaboration with international and local NGOs and other government departments. In 2015, 83 per cent of persons who had enrolled in MMT continued the treatment for at least six months.
The National AIDS Progamme screened 15,859 people living with HIV for TB infection in 2015 (85% [[92%]] of target), across 63 sites including ART centres, decentralized ART sites and TB–HIV collaborative sites.
TB–HIV collaborative activities and coordination significantly improved. The communication from the Global Fund on the need to strengthen collaboration proved very helpful in furthering the collaboration between the two programmes.