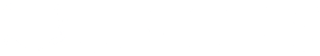
The cumulative results for Year 5 (NFM) are shown as a percentage of the annual target. TB–HIV indicator (collaborative sites) and MDR-TB treatment indicators are funded by GFATM and other donors, while the others are funded by GFATM only.
TB grant implementation has also shown progress with four out of eight reportable indicators either meeting or exceeding the annual targets. TB control service coverage was expanded to 330 townships by early 2015. During the year, 140,699 TB patients were notified and enrolled on treatment (83% of the annual target) of which 47,301 (88%) were bacteriologically confirmed. The treatment success rate among bacteriologically confirmed TB cases was 85 per cent (40,120/47,420).
To increase case notification, coordination has been increased with other service providers such as military hospitals, public and private hospitals, and NGOs in border areas (involving ethnic minority health workers in partnership with SMRU in Kayin).
External quality assurance samples (quality control slides) from 412 of the 447 participating laboratories were sent for assessment, and 385 of the 412 laboratories (93%) met the quality control performance criteria. Training and mentoring of Upper and Lower Myanmar TB Laboratories, technical assistance and supportive supervision by WHO were crucial in achieving this result.
In 2015, 2,793 (73%) MDR-TB cases were notified. Between 2011 and 2015, the number of MDR-TB patients enrolled on treatment increased from 50 to 2,207 cases.
The expansion of TB–HIV activities has been implemented in collaboration with the National AIDS Programme and other partners. During 2015, the HIV test results of 64 per cent (89,350) of notified TB cases were recorded in the TB register, significantly exceeding the programmatic target of 45 per cent. The programme has maintained this high performance since last year. Encouraging individuals to accept HIV counselling and testing services takes time and needs careful communication and trust building. Individuals may initially feel reluctant to be tested but with information and support they often eventually willingly accept HIV counselling and testing.